INVIVOX: Can you give us a historical reminder of deep brain stimulation?
Prof Stéphane Palfi: Deep brain stimulation (DBS) was developed in 1987 at the initiative of Professor Alim Louis Benabid, in Grenoble, who demonstrated that an implanted system with stimulation of the thalamus could have a very satisfactory effect on essential tremor in the long term. Previously, there had been transient intraoperative stimulation performed before the lesion and which showed significant results. No one had previously implemented a device to stimulate patients with neurological diseases in the long term. This technique has been made possible through the development of medical devices such as chronic implanted electrodes and pulse generators.
INVIVOX: Besides Parkinson's, what other diseases is this neurostimulation technique applied to?
Prof Stéphane Palfi: Professor Benabid originally started with patients suffering from severe essential resistant tremor. Quickly after, he made the first applications in Parkinson's disease, then in primary genetic dystonia. Other applications are being evaluated using other targets such as in surgery of obsessive-compulsive disorder (OCD) resistant to medical treatment or severe and disabling Tourette syndrome (tics).
INVIVOX: What are the indications and contraindications?
Prof Stéphane Palfi: We target patients who have forms of disease resistance to medical treatment, or whose medical treatment induces adverse effects. Contraindications to the implantation of intracerebral electrodes are where interrupting anticoagulants is impossible, patients with advanced dementia or other more specific contraindications of a neurological disease.
INVIVOX: What are the prospects for deep brain stimulation?
Prof Stéphane Palfi: The miniaturisation of medical devices, the new rechargeable devices, the increasing capacity for fine tuning of the various parameters, have allowed all these advances. We have reached a stage where we are implanting directional electrodes to direct the electrical stimulation field: a very significant advance which would avoid unwanted effects and improve efficiency. In a few months, based on the recording of the stimulated areas, we will be able to correct the stimulation parameters. And within a year or two, it may be that, depending on the detections made by the recordings in the brain, automatic correction of the stimulation parameters will further improve efficiency. Another important advance: until very recently, we could not do a magnetic resonance imaging (MRI) scan after implantation as there was a risk that the electrode would overheat due to the magnetic field, but devices more compatible with MRI magnetic fields are now available. In parallel, the constant progress in MRI now allows better visualisation of targets to better position the electrode. We also use MRI for quality control and placement of the electrode.
INVIVOX: What is the split between theory and practice in your course?
Prof Stéphane Palfi: The day before going in the operating room, we start the theoretical training with a presentation on all the indications, the history of stimulation, all the surgical procedures in progress and the procedures for patient selection, monitoring and quality control. On the practical side, we train participants to place the stimulation target on a neuronavigation station using imagery of the surgery planned the next day. We also teach the fundamental principles to develop a deep brain stimulation activity within a healthcare structure. In some countries, deep brain stimulation does not yet exist, so it is important to be able to convince national health organisations to develop this therapeutic approach. This training will provide information on all economic and practical aspects to develop this activity. In addition to neurosurgeons, training can be useful for economic decision-makers in health establishments.
INVIVOX: During this training, you insist a lot on patient selection, why?
Prof Stéphane Palfi: If patients are not properly selected, the results will not meet the expectations of patients and practitioners, which can be highly detrimental to the reputation of the technique. Over the 30 years we have been using DBS at Henri Mondor, and with the entire scientific community, we have defined guidelines in order to recruit the right patient profiles who will really benefit from the technique with few undesirable effects.
INVIVOX: What are the complications?
Prof Stéphane Palfi: At the end of the day, when we follow the proper procedures, from patient selection to implantation and monitoring, we encounter very few complications. This treatment is reversible (we can remove the device at any time) but also modular (we can modify the stimulation parameters according to the patient's reaction). Complications are related to surgery, the rarest of which are haemorrhagic (<1%). However, in all intracerebral surgeries, when operational complications arise, these can also be extremely serious. Infections are also possible with a slightly higher ratio, but which can find a favourable terrain in weakened and elderly patients.
INVIVOX: Are there any limits to deep brain stimulation?
Prof Stéphane Palfi: Yes, because we are not going to be able to treat all the symptoms in Parkinson's disease, for example. There are other circuits involved in the disease that cannot be treated with stimulation or medication. As the disease progresses, we will have a little less indirect effectiveness: that is, there will always be some effectiveness, but other symptoms will appear to the point of becoming bothersome but not sensitive to stimulation. It is precisely these symptoms that we are trying to detect because when they are diagnosed very early, they evolve very quickly and, in this case, there is very little point in applying stimulation because the overall benefit will not be significant.
INVIVOX: What do you recommend to neurosurgeons who wish to embark on deep brain stimulation?
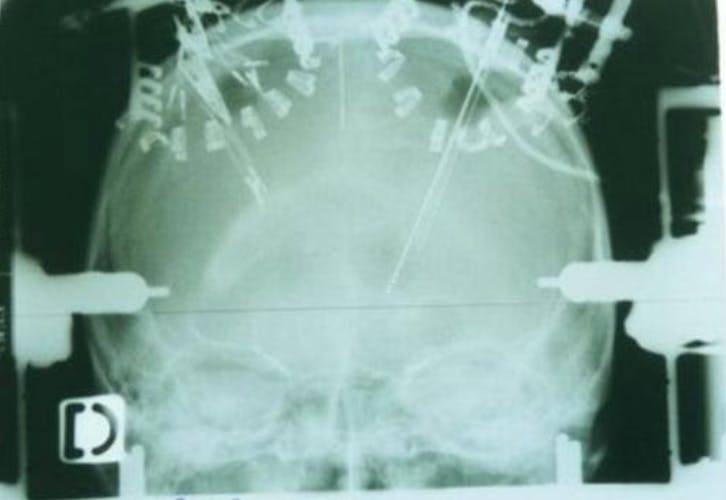
Prof Stéphane Palfi: To train well and to surround themselves with a fully trained and complete team. It is necessary to have complete imaging and stereotaxis equipment in order to have every chance of correctly implanting the intracerebral electrodes.
INVIVOX: In Parkinson's what is the percentage of successes, failures and complications?
Prof Stéphane Palfi: In our department, we improve the clinical scores of Parkinson's disease by 62% on average. We are reducing drug treatments by more than 50% for a better quality of life for our patients.
INVIVOX: You must have your own tips and tricks; can you give us a concrete example that you will share with participants?
Prof Stéphane Palfi: We were the first in France to be equipped with a scanner in the operating room. It allows us to better identify the target and reduce operating times. We operate under general anaesthesia with the help of intraoperative electrophysiology specially designed for GA.
INVIVOX: What benefits will participants gain from this training?
Prof Stéphane Palfi: They will benefit from 30 years of hindsight in deep brain stimulation in one of the largest European centres in psychosurgery with the latest generation equipment. We organise multidisciplinary consultation meetings every Monday, the ultimate goal being that participants who wish to attend will do so remotely.
INVIVOX: What will they be able to do concretely when they get home?
Prof Stéphane Palfi: They will be able to identify and aim at the targets with the correct positioning of the electrodes. They will learn the basics of intraoperative electrophysiological examination. They will however need to attend several trainings to perfect their skills.
INVIVOX: What is the future of stimulation?
Prof Stéphane Palfi: We are currently working a lot on neuromodulation, that is, the modulation of neuron activity by electrical stimulation. Our team is directing its research on stimulation by light. We are genetically modifying the neurons so that they are sensitive to light: depending on the colour (red, yellow, blue ...), the neuron will be activated or inhibited. It is a complex technology under development to better understand the mechanisms of stimulation, better define new targets for electrical stimulation and which may one day be directly applied to treat symptoms of neurological and/or psychiatric diseases.